Discover expert tips and best practices for accurate OASIS documentation to improve compliance, outcomes, and Medicare reimbursement in home health.
Introduction
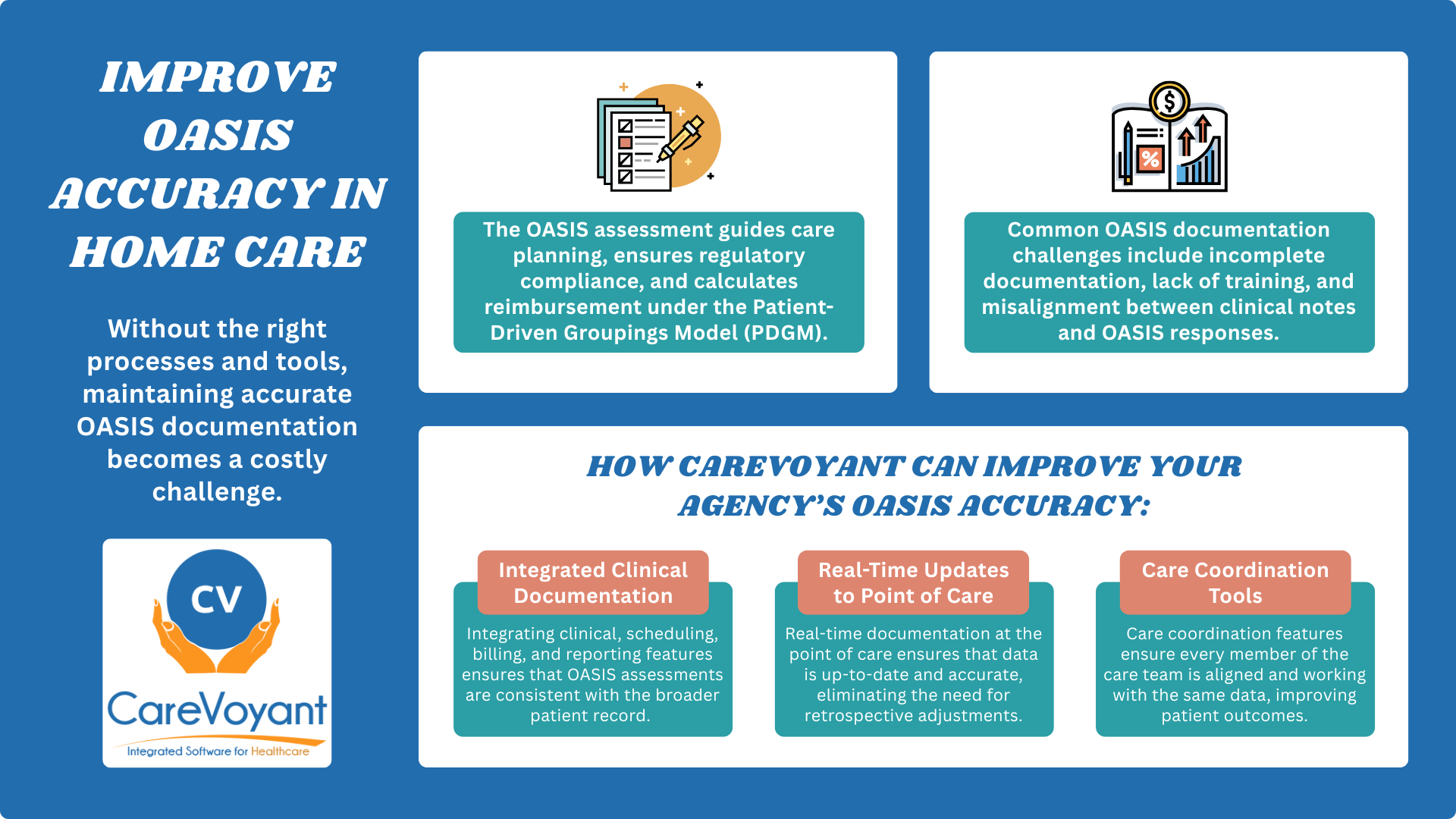
In home health care, managing OASIS assessments accurately is more than a regulatory task—it directly impacts patient outcomes, agency performance, and Medicare reimbursement. The Outcome and Assessment Information Set (OASIS) serves as the clinical foundation for care planning, quality reporting, and PDGM payment calculations. Yet, many agencies struggle with OASIS documentation errors that lead to compliance issues, lost revenue, and poor care quality. Accurate documentation helps improve scores on Home Health Compare and Star Ratings, which patients and families use to evaluate agencies. Without the right processes and tools, maintaining accurate OASIS documentation becomes a costly challenge. This guide shares proven OASIS assessment best practices to help home health agencies ensure accuracy, improve outcomes, and stay Medicare-compliant.
What Is the OASIS Assessment?
The OASIS assessment—short for Outcome and Assessment Information Set—is a standardized data collection tool required by the Centers for Medicare & Medicaid Services (CMS) for all Medicare-certified home health agencies. Its primary purpose is to measure patient outcomes, guide care planning, ensure regulatory compliance, and calculate reimbursement under the Patient-Driven Groupings Model (PDGM).
There are several types of OASIS assessments, each corresponding to key events in a patient’s care journey:
Start of Care (SOC) – when services begin
Resumption of Care (ROC) – after a hospital stay or inpatient facility discharge
Recertification – completed every 60 days if services continue
Transfer – when a patient transitions to another facility or care level
Discharge – upon completion of services
Death at Home – when applicable
Each assessment provides updated clinical, functional, and service-related data, which is vital for tracking progress and maintaining continuity of care.
OASIS documentation must be completed by qualified clinicians—typically a Registered Nurse (RN), Physical Therapist (PT), Speech-Language Pathologist (SLP), or Occupational Therapist (OT), depending on the discipline initiating care. Accurate and timely completion is essential for proper care delivery and payment integrity.
Importantly, OASIS data directly influences Home Health Resource Group (HHRG) classification, which drives PDGM reimbursement. Inaccuracies can lead to underpayments, compliance risks, and skewed outcome reporting. That is why accurate OASIS documentation is not just an administrative task; it is a critical component of operational success in home health care.
Common Challenges in OASIS Documentation
Even the most experienced home health clinicians can struggle with the complexity of OASIS documentation. Below are some of the most common challenges agencies face, each of which can significantly impact home health OASIS accuracy and Medicare compliance.
Inconsistent or Incomplete Clinical Documentation
One of the most frequent issues is the lack of detailed, objective clinical documentation. When notes are vague or missing key information, it becomes difficult to justify OASIS responses, leading to inaccuracies that affect care quality and reimbursement.
Lack of Training or Understanding of OASIS Questions
OASIS-E assessments are complex and regularly updated. Clinicians without proper, ongoing training may misinterpret scoring criteria, especially functional or cognitive items—resulting in errors that can impact quality reporting and PDGM reimbursement.
Rushed or Late Assessments
Time constraints, staffing shortages, or workflow inefficiencies often cause assessments to be completed hastily or submitted late. This not only compromises the accuracy of OASIS documentation but may also lead to CMS non-compliance or penalties.
Communication Gaps Between Interdisciplinary Teams
Poor communication between nurses, therapists, and other team members can lead to conflicting documentation. Without alignment on patient status, OASIS responses may be inconsistent with clinical observations and care plans.
Misalignment Between Clinical Notes and OASIS Responses
Perhaps the most serious challenge is when clinical documentation does not match the selected OASIS items. For example, if a patient's mobility limitations are detailed in the narrative but marked as "independent" in the OASIS, it creates compliance risks and may trigger audits.
Overcoming these challenges is key to achieving accurate OASIS documentation, improving patient outcomes, and ensuring financial sustainability for home health agencies. Agencies must follow Medicare’s Conditions of Participation for home health agencies to stay compliant and eligible for reimbursement.
How Home Health Software Streamlines OASIS Documentation
In the high-stakes world of home health care, accurate OASIS documentation is the key to regulatory compliance, optimal reimbursement, and improved patient outcomes. With complex assessment requirements and evolving CMS regulations, manual or disjointed workflows often lead to errors, delays, and audit risks. That is where robust CareVoyant home health software solutions come in—streamlining OASIS workflows, improving accuracy, and empowering clinicians with real-time tools and insights.
Integrated Clinical Documentation for OASIS Accuracy
CareVoyant Home Health Software offers an all-in-one platform that integrates clinical, scheduling, billing, and reporting features—ensuring that OASIS assessments are consistent with the broader patient record. Rather than working in silos, clinicians can complete documentation, review care plans, and access historical data in one place.
This integration addresses a common challenge in home health: the misalignment between clinical notes and OASIS responses. With CareVoyant’s structured templates and validation logic, clinicians are guided through the OASIS-E assessment with prompts and alerts that flag inconsistencies or missing data. This helps agencies ensure accurate OASIS documentation aligns with CMS standards and internal clinical records.
Real-Time Point-of-Care Documentation
One of the leading causes of OASIS errors is delayed or rushed documentation. CareVoyant solves this with powerful point-of-care (POC) capabilities that allow clinicians to complete OASIS assessments on tablets or mobile devices during patient visits.
This real-time documentation ensures that data is fresh, accurate, and entered in context. It eliminates the need for retrospective updates that may rely on memory or incomplete notes. CareVoyant’s smart interface provides immediate feedback if entries are out of range, incomplete, or inconsistent—helping clinicians correct issues before submission and reducing the risk of CMS audit triggers.
Clinical Decision Support & Validation Tools
CareVoyant is equipped with clinical decision support features that assist clinicians throughout the OASIS process. Built-in rules help standardize responses, especially for functional and cognitive scoring, which are often prone to variability due to inconsistent clinician training or interpretation.
As clinicians input responses, the system cross-references clinical documentation, diagnosis codes, and prior assessments to guide accurate entries. This reduces discrepancies and promotes compliance with PDGM and quality reporting requirements. For agency administrators, these tools offer peace of mind that every assessment is both thorough and justifiable.
Interdisciplinary Communication Support
Communication gaps between clinicians, therapists, and care coordinators can lead to fragmented or contradictory documentation. CareVoyant addresses this challenge with real-time access to shared patient records, secure messaging, and team collaboration features. This functionality ensures that every member of the care team is aligned and working from the same up-to-date clinical data, eliminating confusion during OASIS documentation, and promoting continuity of care.
Clinicians can also reference prior OASIS responses, view scheduled tasks, and coordinate follow-ups directly from the CareVoyant interface, minimizing miscommunication and redundant data entry.
Productivity Tools that Improve Clinician Utilization
CareVoyant does not just streamline documentation, it makes clinicians more productive. The software includes intuitive dashboards, automatic population of recurring data, and pre-filled patient information that significantly reduces manual entry time. These features allow clinicians to focus more on patient care and less on paperwork.
By enhancing clinician utilization, agencies reduce burnout, ensure timely completion of OASIS assessments, and boost overall accuracy. This helps solve common challenges like rushed or late assessments and staff documentation fatigue, both of which can compromise compliance and quality.
Conclusion
Effectively managing OASIS assessments is vital for every home health agency striving to deliver high-quality care, remain compliant with CMS regulations, and optimize reimbursement under PDGM. From ensuring accurate functional scoring to maintaining consistent clinical documentation, every aspect of the OASIS process plays a critical role in patient outcomes and agency performance.
To overcome common challenges—such as inconsistent documentation, communication gaps, and rushed assessments—agencies must adopt a proactive strategy grounded in training, process standardization, and most importantly, the right technology. Investing in an all-in-one solution, CareVoyant Home Health Software not only streamlines OASIS documentation but also enhances real-time decision-making, interdisciplinary collaboration, and overall clinical efficiency.
Success in OASIS documentation requires a balance of technology, empathy, and accuracy. While CareVoyant software delivers intelligent tools and automation, it is the combination of those capabilities with compassionate, well-trained clinicians that drive meaningful outcomes.
By committing to continuous quality improvement and leveraging purpose-built CareVoyant real-time point-of-care tools, home health agencies can transform OASIS from a regulatory burden into a strategic asset—ensuring better care, stronger compliance, and sustainable growth.
Frequently Asked Questions
-
OASIS documentation refers to the standardized clinical assessments home health agencies must complete to measure patient outcomes, ensure Medicare compliance, and determine reimbursement under PDGM.
-
Accurate OASIS documentation ensures proper care planning, affects PDGM reimbursement rates, supports CMS compliance, and directly impacts patient outcomes and agency star ratings.
-
Qualified clinicians such as Registered Nurses (RNs), Physical Therapists (PTs), Speech-Language Pathologists (SLPs), and Occupational Therapists (OTs) complete OASIS assessments depending on the initiating discipline.
-
OASIS assessments include Start of Care (SOC), Resumption of Care (ROC), Recertification, Transfer, Discharge, and Death at Home, based on specific patient care events.
-
OASIS responses help determine the Home Health Resource Group (HHRG), which CMS uses to calculate reimbursement under the Patient-Driven Groupings Model (PDGM).
-
Common OASIS documentation errors include incomplete clinical notes, misinterpreted assessment items, late submissions, and misalignment between narrative documentation and selected responses.
-
CareVoyant Home health care software improves OASIS accuracy through real-time documentation, built-in validation rules, point-of-care access, and decision support tools.
-
Effective software for OASIS should offer integrated clinical workflows, point-of-care access, auto-validation, interdisciplinary communication tools, and compliance-ready templates.
-
OASIS must be completed at admission (SOC), every 60 days for recertification, after hospitalizations (ROC), at discharge, or during significant care transitions.
-
Ongoing training using real case scenarios, OASIS-E updates, software simulations, and CMS-aligned resources is the best way to improve clinician confidence and documentation accuracy.
About CareVoyant
CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home based services, including Home Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services (HCBS), Home Health, Pediatric Home Care, and Outpatient Therapy at Home.
CareVoyant functions – Intake, Authorization Management, Scheduling, Clinical with Mobile options, eMAR/eTAR, Electronic Visit Verification (EVV), Billing/AR, Secure Messaging, Notification, Reporting, and Dashboards – streamline workflow, meet regulatory requirements, improve quality of care, optimize reimbursement, improve operational efficiency and agency bottom line.
For more information, please visit CareVoyant.com or call us at 1-888-463-6797.
Request for Information
To learn more about CareVoyant Software and how we improve the operational efficiency of Home Healthcare Agencies, contact us: