Poor authorization management leads to denied claims, compliance risks, and care disruptions. Automating authorizations through CareVoyant’s integrated home care software helps agencies protect revenue, ensure compliance, and maintain uninterrupted patient care.
Introduction
Authorization management has become one of the most critical and easily overlooked administrative responsibilities in today’s home health and personal care environment. With strict payer requirements outlined by the Centers for Medicare & Medicaid Services (CMS) and complex rules across Medicaid waiver programs, agencies are under constant pressure to track authorization dates, units, and care plan changes with absolute precision.
When authorizations expire unnoticed, exceed approved limits, or fail to align with the plan of care, the consequences are far-reaching. Research from the Agency for Healthcare Research and Quality (AHRQ) shows that disruptions in care coordination can negatively impact patient outcomes, while authorization-related billing errors frequently trigger audit findings reported by the HHS Office of Inspector General (OIG).
This article explores the true financial, clinical, and compliance risks of authorization mismanagement and how CareVoyant’s integrated Home Care Software helps agencies prevent denials, protect revenue, and deliver uninterrupted, high-quality care.
The Real Cost of Authorization Errors
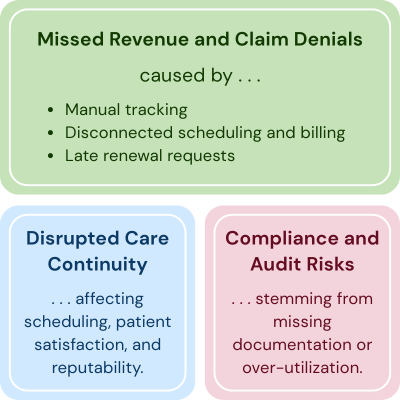
1. Missed Revenue and Claim Denials
Even a single missed authorization renewal or over-scheduled visit can lead to denied claims. When staff deliver services outside of an approved authorization window or exceed the allowed units, payers reject those visits resulting in direct revenue loss.
Common causes:
Manual tracking of authorization dates and units
Disconnected scheduling and billing systems
Late renewal requests to payers
Each denied claim represents hours of unpaid care and administrative time spent on rework.
2. Disrupted Care Continuity
Expired authorizations can cause sudden service interruptions. Field staff may arrive for a scheduled visit only to find that the authorization has expired or doesn’t cover the needed care. This not only affects patient satisfaction but can also damage your agency’s reputation with referral sources and payers.
3. Compliance and Audit Risks
Payers, especially Medicaid and Managed Care Organizations (MCOs), require strict adherence to authorization terms. Missing documentation or over-utilization can lead to compliance findings during audits, repayment demands, or even exclusion from preferred provider networks.
Why Authorization Management Fails in Many Agencies
Most home care agencies struggle with one or more of these systemic issues:
Data Silos: Authorization details live separately in intake forms, spreadsheets, and billing systems.
Lack of Automation: No automatic alerts for expiring or exceeded authorizations.
Poor Visibility: Staff across scheduling, billing, and clinical teams don’t see real-time authorization data.
Manual Reconciliation: Matching authorized units to billed visits is slow and error prone.
Without automation and integration, the risk of error grows exponentially as patient volume increases.
How CareVoyant Home Care Software Solves the Authorization Challenge
CareVoyant’s Authorization and Plan of Care Management module helps home care agencies simplify one of their toughest operational areas, managing payer authorizations accurately while ensuring compliance and continuity of care.
Here’s a detailed look at how each feature works and how it transforms your daily workflow.
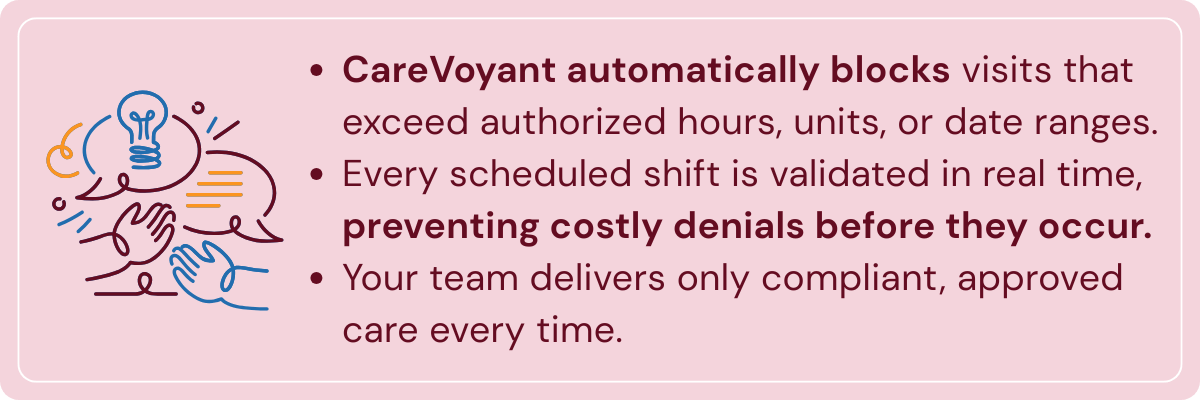
1. Prevents Scheduling Beyond Authorized Limits
One of the biggest pain points for home care agencies is unintentional overscheduling when staff unknowingly book visits that exceed the number of hours or units approved by the payer. These errors often lead to claim denials, compliance risks, and lost revenue.
CareVoyant’s scheduling system automatically validates every scheduled visit against the client’s current authorization. If a caregiver tries to schedule beyond the approved limit or outside the authorization date range, the system flags it instantly.
This real-time control ensures that only compliant, authorized visits are delivered. The result: fewer denied claims, accurate visit capture, and consistent compliance across all payer programs. For how scheduling links to authorization, see scheduling efficiency and authorization management.
2. Proactive Alerts for Expiring Authorizations and Care Plans
Authorization expirations can cause serious disruptions in care delivery and billing if not renewed in time. CareVoyant prevents this by generating proactive alerts and notifications before an authorization or plan of care expires.
Administrators and care coordinators receive early warnings based on configurable lead times for example, 15 or 30 days before expiration, allowing them to start renewal processes well in advance.
This foresight ensures that care continues seamlessly, without last-minute scrambling or gaps in coverage. Agencies benefit from uninterrupted service delivery, timely renewals, and stronger compliance with payer requirements. Pair alerts with our authorization management best practices.
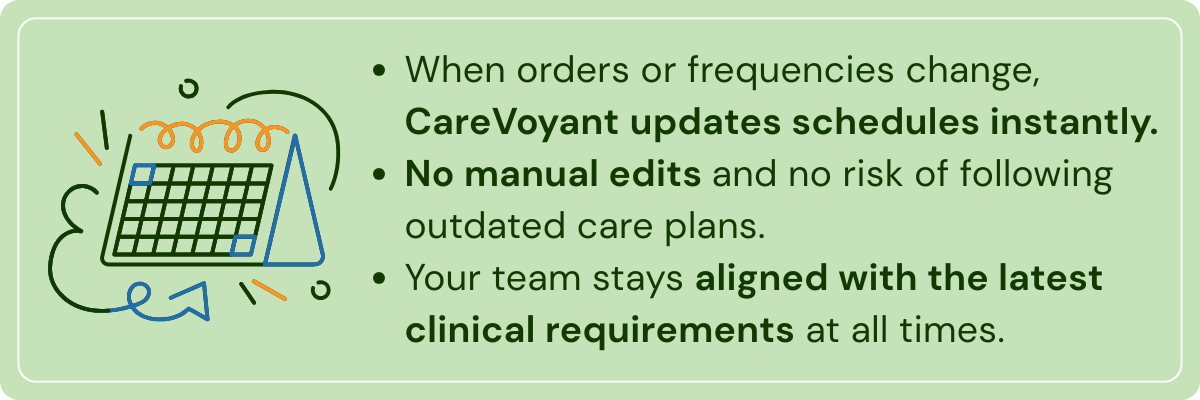
3. Automatic Schedule Updates When Plans of Care Change
Care plans evolve frequency, duration, or order details often change mid-authorization. Manually updating schedules to reflect these changes can be tedious and error prone.
CareVoyant eliminates that risk by automatically synchronizing schedules whenever the plan of care is modified. When a clinician updates service frequency or duration in the system, all related schedules adjust automatically to align with the new plan.
This feature ensures that care staff always follow the latest physician orders, maintaining plan-of-care compliance while saving administrative staff from hours of manual rescheduling. It’s a simple but powerful way to keep care delivery and documentation in sync. For clinical documentation best practices that pair well with this, read home health documentation & Medicare compliance.
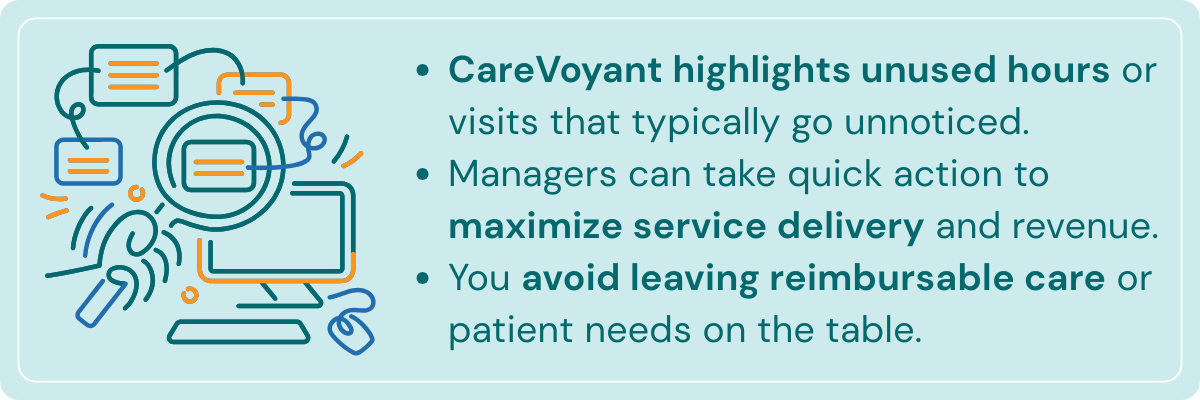
4. Tracks Underutilized Authorizations
In many agencies, staff focus so much on avoiding overuse that they overlook underutilized authorizations unused visits or hours that represent missed opportunities and lost revenue.
CareVoyant continuously tracks utilization and highlights authorizations that are falling behind expected usage. Managers can quickly identify clients whose visits are below authorized levels and take corrective actions, such as scheduling make-up visits or reassessing service frequency.
This visibility helps agencies maximize revenue potential while ensuring clients receive the full scope of approved care. It’s not just about preventing over-delivery, it’s also about making sure you don’t leave approved hours unclaimed. Related reading: optimize staff utilization with intelligent scheduling.
5. Integrates Authorization Data Across Scheduling, Billing, and Clinical
One of CareVoyant’s most powerful strengths is its end-to-end integration. Authorization information flows seamlessly through every part of the care process from intake and scheduling to clinical documentation and billing.
Schedulers see authorization limits in real time, clinicians document against approved visits, and billing staff automatically submit claims that match payer authorizations. There’s no need for duplicate data entry or manual reconciliation between systems.
This unified workflow eliminates silos, improves data accuracy, and ensures that everyone from front-line caregivers to back-office teams work from the same verified source of truth. The result is cleaner claims, fewer errors, and faster reimbursements. See reduce unbilled claims and improve cash flow for RCM tie-ins.
6. Supports Multiple Payer Types
Every payer has different authorization formats, renewal rules, and approval requirements and managing them manually can overwhelm even the most organized agencies.
CareVoyant is designed to handle multiple payer types and funding sources within ONE integrated platform. Whether you’re managing clients under Medicaid waiver programs, private insurance, managed care organizations, or blended funding, CareVoyant adapts to each payer’s unique structure.
You can define payer-specific authorization templates, automate renewals, and apply different service rules without juggling separate systems. This flexibility allows agencies to expand into new payer contracts or programs without increasing administrative workload.
By centralizing all payer workflows in one place, CareVoyant makes multi-payer management simple, consistent, and scalable. For strategies to expand the services and diversify the payers that pair well with this, read Payer diversification strategies.
Conclusion
Authorization management has traditionally been viewed as a back-office task. But in reality, it’s one of the biggest levers for improving financial performance and care quality.
By moving from manual tracking to automated, integrated authorization workflows, home care agencies can:
Protect revenue by preventing denials
Ensure compliance with payer requirements
Improve efficiency through data-driven automation
Deliver uninterrupted care for every patient
With CareVoyant Home Care Software, home care agencies can finally stay ahead of the curve, transforming a daily administrative burden into a powerful, strategic advantage.
Frequently Asked Questions
-
Authorization management in home care is the process of tracking payer-approved services, including authorized dates, units, and visit limits, to ensure care delivery aligns with payer requirements and is reimbursable.
-
Authorization mismanagement can lead to denied claims, lost revenue, compliance violations, and care interruptions when services are delivered outside approved limits or after authorizations expire.
-
When authorizations expire unnoticed, payers deny claims for services already delivered, forcing agencies to absorb unpaid care costs and spend additional time on rework and appeals.
-
Yes. Medicaid, MCOs, and other payers require strict adherence to authorization terms. Over-utilization, missing documentation, or expired authorizations can trigger audit findings, repayment demands, or network exclusion.
-
Common causes include manual tracking methods, disconnected scheduling and billing systems, lack of automated alerts, data silos, and limited visibility across clinical, scheduling, and billing teams.
-
CareVoyant automatically validates every scheduled visit against the client’s active authorization, flagging or blocking visits that exceed approved units, hours, or date ranges before they occur.
-
Proactive alerts notify staff well before authorizations or plans of care expire, allowing renewals to be requested early and preventing last-minute service disruptions or gaps in patient care.
-
Without automation, plan-of-care changes can lead to outdated schedules and noncompliant visits. CareVoyant automatically updates schedules to match revised orders, frequencies, or durations.
-
Underutilized authorizations represent missed revenue and incomplete care delivery. Tracking unused hours or visits helps agencies maximize approved services while ensuring patients receive their full scope of care.
-
CareVoyant Integrated home care software centralizes authorization data across scheduling, clinical documentation, and billing, eliminating silos, reducing errors, improving compliance, and accelerating reimbursement.
About CareVoyant
CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home based services, including Home Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services (HCBS), Home Health, Pediatric Home Care, and Outpatient Therapy at Home.
CareVoyant functions – Intake, Authorization Management, Scheduling, Clinical with Mobile options, eMAR/eTAR, Electronic Visit Verification (EVV), Billing/AR, Secure Messaging, Notification, Reporting, and Dashboards – streamline workflow, meet regulatory requirements, improve quality of care, optimize reimbursement, improve operational efficiency and agency bottom line.
For more information, please visit CareVoyant.com or call us at 1-888-463-6797.
Request for Information
To learn more about CareVoyant Software and how we improve the operational efficiency of Home Healthcare Agencies, contact us: