Hospital-at-Home (HaH) programs are reshaping healthcare by delivering hospital-level care in the home. Non-medical home care providers can play a vital role in improving recovery, reducing readmissions, and enhancing patient satisfaction, if they build the right partnerships, technology, and operational readiness.
Introduction
Hospital-at-Home (HaH) programs are gaining traction as hospitals face overcrowding, rising costs, and patient demand for home recovery. Evaluations show HaH models yield lower mortality, fewer complications, and up to 19% cost savings.
Non-medical home care providers are essential for daily support, environmental management, and care continuity, functions that clinical teams alone cannot cover. This article explores HaH’s landscape, the value of non-medical support, and how agencies can strategically position themselves for success.
Understanding the HaH Model
HaH delivers acute-level medical treatment at home, replicating hospital care with physician oversight, nursing, diagnostics, and therapies. Its success depends on integrating clinical components (medication management, monitoring) with non-clinical supports (personal care, meals, home safety).
Since COVID-19, CMS’s Acute Hospital Care at Home waiver has accelerated adoption. Studies indicate HaH reduces readmissions by 26% and cuts costs by 19-30%, while improving patient satisfaction (NEJM).
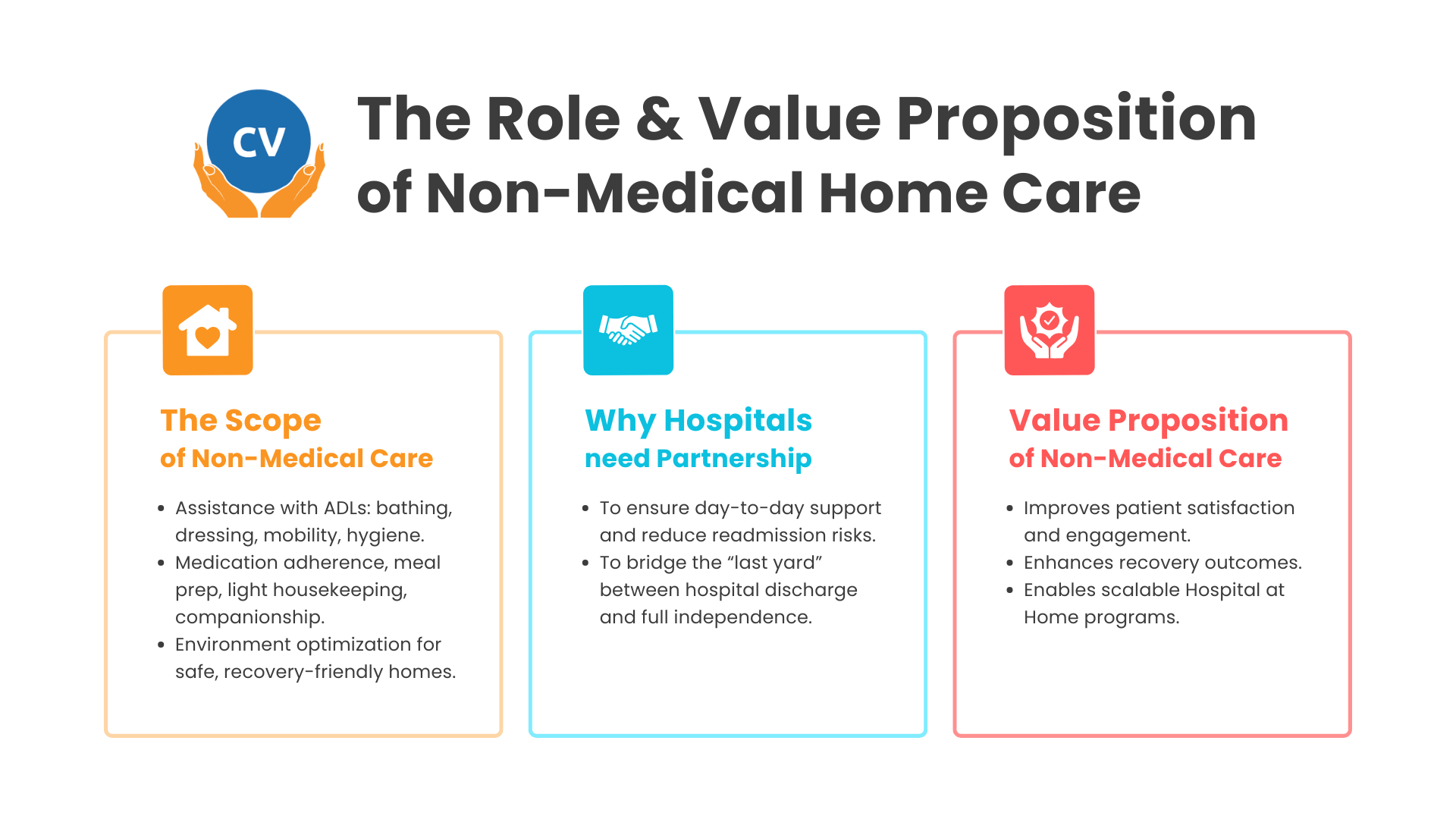
The Role & Value Proposition of Non-Medical Home Care
The Scope of Non-Medical Care:
Assistance with ADLs: bathing, dressing, mobility, hygiene.
Medication adherence, meal prep, light housekeeping, companionship.
Environment optimization for safe, recovery-friendly homes.
Why Hospitals Need Non-Medical Partners:
Ensure day-to-day support and reduce readmission risks.
Bridge the “last yard” between hospital discharge and full independence.
Non-Medical Care Value Proposition:
Improves patient satisfaction and engagement.
Enhances recovery outcomes.
Enables scalable HaH programs.
HaH Opportunity Landscape & Market Trends
Current Adoption: 366 hospitals in 39 states participated in AHCAH by 2024, treating over 31,000 patients (MedPAC).
Medicaid Inclusion: 12 states reimburse HaH under Medicaid, though uptake varies due to waiver uncertainty (CHCS).
Growth Drivers: Aging population, chronic conditions, improved remote monitoring, cost pressures on hospitals (American Medical Association).
Risks: Regulatory uncertainty, hospital trust, liability, staffing, and geographic dispersion.
Competitive Landscape: Traditional home health agencies, non-medical providers, concierge HaH services, and in-house hospital HaH programs (American Hospital Association).
4 Strategic Entry Paths for Non-Medical Home Care Providers
Hospital Partnerships: Subcontracted or joint venture models to provide non-clinical support.
Managed Care & ACO Integration: Align non-medical support with value-based care metrics.
Bundled Payments & Shared Savings: Participate in financial models tied to outcomes.
Pilots & Proof-of-Concept Programs: Use small-scale programs to demonstrate impact and build partnerships.
Operational Readiness for Hospital-at-Home Success
To successfully participate in Hospital-at-Home (HaH) programs, non-medical home care providers must ensure operational readiness across people, processes, and technology. Effective integration with hospitals and payers requires not only clinical alignment but also digital interoperability, real-time visibility, and compliance-driven workflows.
Below are six core operational capabilities and how CareVoyant’s integrated Personal Care Software enables home care agencies to meet and exceed these expectations.
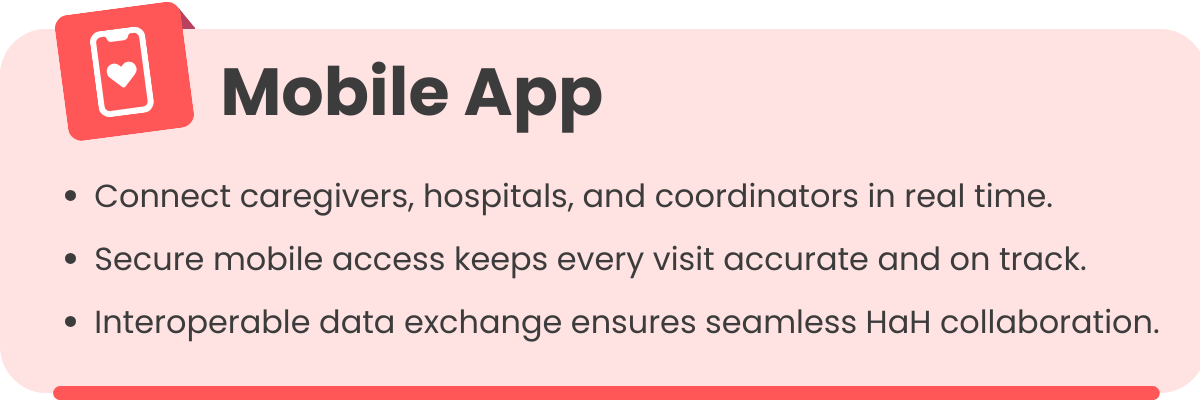
1. Mobile Care Apps, Secure Communication & Interoperable Data Exchange
Challenge: HaH requires caregivers, clinical teams, and hospital coordinators to exchange information instantly. Delays or errors in communication can compromise patient safety.
Impact: Missed updates or miscommunications can result in delayed interventions, readmissions, or medication errors.
CareVoyant Solution: CareVoyant’s EVV and CV Mobile platform offers HIPAA-compliant, mobile access to care plans, visit details, and documentation. Caregivers can report patient vitals or symptom changes in real time, automatically notifying hospital teams. Through Care Coordination & Communication tools, agencies centralize patient information, reducing errors and improving continuity across multidisciplinary teams.
For a deeper look at how improved collaboration enhances outcomes, read Enhancing Care Team Communication to Improve Quality of Care.
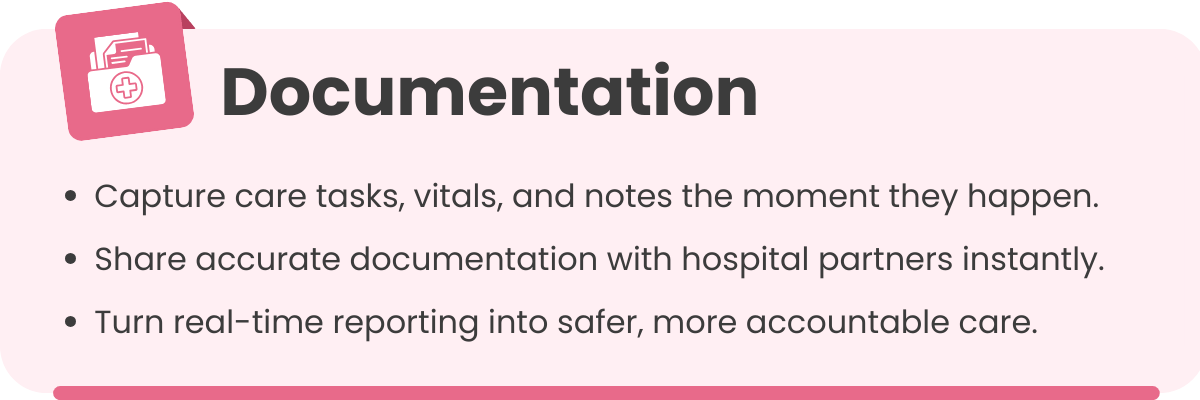
2. Documentation, Reporting & Data Sharing Protocols
Challenge: Accurate documentation is critical for patient safety, compliance, and reimbursement.
Impact: Incomplete or delayed records increase the risk of medication errors, noncompliance, and denied claims.
CareVoyant Solution: CareVoyant’s Clinical and Point-of-Care module allows caregivers to document visits in real time, capturing tasks, vitals, and observations. Integrated eMAR/eTAR ensures accurate medication administration and treatment tracking. Additionally, Reports and Dashboards provide actionable insights into service utilization, patient progress, and compliance metrics, which can be shared securely with hospital administrators or payers.
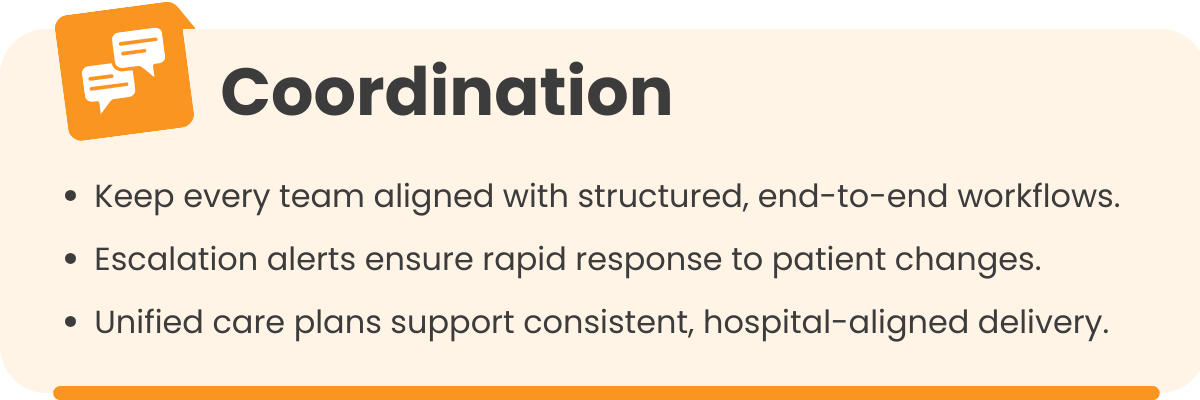
3. Coordination & Care Workflows
Challenge: HaH models demand tight coordination between medical and non-medical teams to maintain continuity of care.
Impact: Fragmented workflows can lead to missed visits, delayed escalations, and inconsistent patient monitoring.
CareVoyant Solution: Authorization and Plan of Care Management ensures all caregivers follow individualized, hospital-approved plans. Real-time alerts allow caregivers to flag issues such as missed medications, safety hazards, or patient decline, triggering escalation to clinical contacts. Structured workflows streamline handoffs, reduce errors, and reinforce accountability.
4. Scheduling, Routing & Responsiveness
Challenge: Home-based acute care requires flexible scheduling and rapid response to changes in patient condition.
Impact: Inefficient scheduling can increase missed visits, caregiver burnout, and patient risk.
CareVoyant Solution: CareVoyant's Home Care Scheduling automates visit assignments, optimizes routes, and adapts to variable visit frequencies. Agencies can match caregivers to patients based on skills, proximity, and availability, ensuring faster response times and consistent care.
As highlighted in Scheduling Efficiency for HCBS and Private Duty Non-Medical Home Care Agencies, CareVoyant helps agencies reduce missed visits, minimize travel time, and improve caregiver productivity, all critical for consistent HaH service delivery.
5. Billing, Reimbursement & Administrative Capabilities
Challenge: Financial sustainability in HaH programs depend on accurate, timely billing and reimbursement.
Impact: Manual processes can lead to claim denials, revenue loss, and administrative inefficiency.
CareVoyant Solution: Billing, A/R, and Revenue Cycle Management automate claim submissions, track payer authorizations, and reconcile revenue across funding sources. Integration with Payroll and Accounting ensures accurate caregiver compensation and transparent cost tracking.
For more insights, see Keys to Effective Revenue Cycle Management for Home Care, a practical guide to improving cash flow and compliance.
6. Risk Management, Liability & Safety Protocols
Challenge: Home-based acute care carries risks that must be proactively monitored and mitigated.
Impact: Delayed detection of incidents or missed services can compromise patient safety and agency compliance.
CareVoyant Solution: Integrated Operational Efficiency dashboards track KPIs like missed visits, patient incidents, and care compliance in real time. Role-based access and audit trails strengthen data security, while automated alerts allow administrators to mitigate risks proactively.
To learn how home care agencies can use data to improve safety and compliance, explore Care Coordination Tools for Home Health Care Agencies.
Conclusion
By unifying intake, scheduling, clinical documentation, communication, billing, and reporting into one connected system, CareVoyant gives non-medical home care agencies the infrastructure they need to operate effectively within Hospital-at-Home ecosystems. From real-time coordination and secure data exchange to automated billing and outcome reporting, CareVoyant enables providers to:
Integrate seamlessly with hospitals and payers.
Deliver consistent, high-quality non-medical support.
Demonstrate measurable impact on recovery outcomes and patient satisfaction.
In essence, CareVoyant’s Personal Care Software empowers agencies to evolve from traditional personal care providers into strategic partners in the future of home-based acute care.
Frequently Asked Questions
-
They support daily living activities, meal prep, home safety, companionship, and monitoring that clinical teams cannot provide consistently.
-
Non-medical caregivers reduce readmission risks, ensure patient safety, and support recovery between clinical visits.
-
Yes. Hospitals frequently partner with personal care agencies for ADL assistance, safety support, and continuous monitoring.
-
Agencies need mobile care apps, secure communication tools, real-time documentation, EVV, scheduling automation, and interoperable data sharing.
-
Accurate documentation ensures patient safety, supports clinical decision-making, prevents medication errors, and strengthens reimbursement compliance.
-
CareVoyant provides mobile documentation, alerts, scheduling automation, billing tools, and interoperable data exchange to coordinate with hospitals.
-
Common challenges include workflow alignment with hospitals, staffing for rapid response, documentation accuracy, and adherence to safety protocols.
-
They provide hands-on support with mobility, hygiene, nutrition, safety, and medication reminders improving recovery and patient experience.
-
Yes. Agencies can participate in ACOs, managed care programs, and shared-savings models when they demonstrate measurable outcome improvements.
-
Hospitals look for agencies with proven operational readiness, technology integration, reliable staffing, and strong quality and safety track records.
About CareVoyant
CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home based services, including Home Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services (HCBS), Home Health, Pediatric Home Care, and Outpatient Therapy at Home.
CareVoyant functions – Intake, Authorization Management, Scheduling, Clinical with Mobile options, eMAR/eTAR, Electronic Visit Verification (EVV), Billing/AR, Secure Messaging, Notification, Reporting, and Dashboards – streamline workflow, meet regulatory requirements, improve quality of care, optimize reimbursement, improve operational efficiency and agency bottom line.
For more information, please visit CareVoyant.com or call us at 1-888-463-6797.
Request for Information
To learn more about CareVoyant Software and how we improve the operational efficiency of Home Healthcare Agencies, contact us: